For decades, dental professionals have been trained to focus on well-known pathogens—Porphyromonas gingivalis, Streptococcus mutans, Fusobacterium nucleatum. These microbes have been extensively studied in relation to caries and periodontal disease. But the more we learn about the oral microbiome, the more it becomes clear that individual pathogens are only part of the picture.
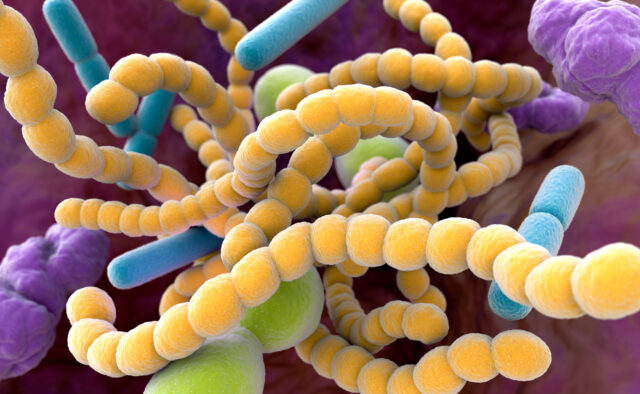
Recent advancements in next-generation sequencing have uncovered a hidden world of bacteria we previously couldn’t study, what microbiologists call “microbial dark matter.” And the most intriguing of these newly discovered microbes? Saccharibacteria, formerly known as TM7.
This tiny, elusive bacterial group is rewriting what we know about oral microbiology. It doesn’t behave like traditional bacteria. It can’t survive alone. It lives on the surface of other bacteria, influencing inflammation and potentially playing a role in both oral health and disease. The implications for periodontology, microbiome-based therapies, and even systemic health are enormous. Let’s dive into what this means for the future of dentistry.
The Bacteria That Lives on Bacteria
So, what makes TM7 unique? Unlike most bacteria, which are free-living or form biofilms, TM7 is an “episymbiont.” This means it attaches to and relies on other bacteria, particularly Actinomyces, to survive. Until 2014, no one had been able to culture TM7 in a lab, making it a complete mystery.
When researchers finally grew it, they were shocked: it behaved almost like a bacterial parasite. Instead of simply coexisting with its host, TM7 seemed to suppress or manipulate Actinomyces. This raised a major question: is TM7 friend or foe?
TM7 in Periodontal Disease
Early studies linked TM7 with inflammation in conditions like periodontitis, vaginosis, and inflammatory bowel disease (IBD). Naturally, researchers assumed TM7 was pathogenic. However, new findings suggest that TM7 might actually help control inflammation rather than cause it.
In a periodontal disease model, researchers introduced Actinomyces into the gums of mice, triggering inflammation and bone loss—just like in human periodontitis. But when TM7 was also introduced, the inflammation decreased, and bone loss was significantly reduced.
This suggests that TM7 might regulate its host bacteria, preventing excessive inflammation and helping to maintain microbial balance. If this holds true in humans, TM7 could have major therapeutic potential.
Could TM7 Be the Key to Future Treatments?
The discovery of TM7’s anti-inflammatory potential opens new doors for dentistry. Imagine if we could harness this bacteria to:
- Reduce periodontal inflammation naturally, without antibiotics or antiseptics.
- Develop probiotics that introduce beneficial TM7 strains to high-risk patients.
- Enhance colonization resistance, using TM7 to outcompete pathogenic bacteria.
We’re already seeing similar microbiome-based therapies in gastroenterology, where fecal transplants and bacterial therapies are being explored for conditions like Crohn’s disease. Dentistry could be next.
What This Means for Your Practice
While TM7 research is still in its infancy, here’s what you should keep in mind:
- Oral health is more than just fighting “bad bacteria.” Microbial ecosystems are complex, and disrupting them with broad-spectrum antimicrobials may have unintended consequences.
- The future of periodontal therapy may involve bacteria, not just antibiotics. TM7-based treatments could eventually help regulate inflammation and prevent disease progression.
- Microbiome science is rapidly evolving. Staying informed about these discoveries will be crucial for integrating new, evidence-based treatments into dental practice.
TM7 challenges everything we thought we knew about oral microbiology. It is neither purely pathogenic nor purely beneficial; its role depends on context, microbial interactions, and host factors. As research progresses, TM7 could become a key player in next-generation periodontal treatments, probiotic therapies, and microbiome-driven approaches to dentistry. Microbial dark matter is a new frontier, and dentists will play a crucial role in exploring its potential.
Dentistry 411 will continue to track the science, the products, and the legal landscape so you don’t have to. Subscribe to stay ahead of the curve, cut through the marketing, and make smarter decisions in your dental practice.